What is Colorectal Cancer
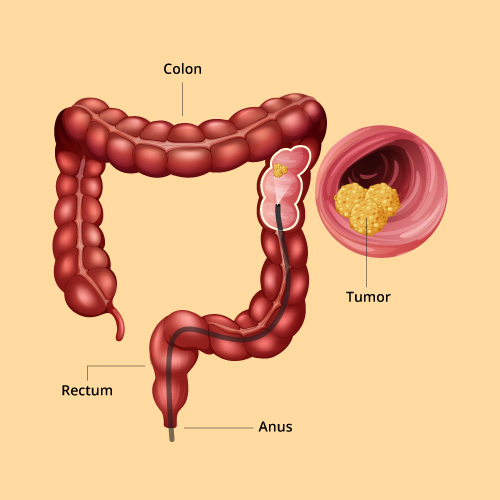
Colorectal cancer also called as cancer of the large intestine,occurs when the cells that line the colonor the rectum become abnormal and grow out of control.
Most cases of colorectal cancer begin as small, noncancerous (benign) clumps of cells called adenomatous polyps. Over time some of these polyps may turns cancerous. By colonoscopy colon cancer and polyps can be visualized.
Incidence
- The incidence of rectal cancer in India is lower than that in the western countries, and it is the tenth leading cancer in India.
- Mean age of rectal cancer (RC): around 40-45 years.
Most common forms of inherited colon cancer syndromes

Hereditary Nonpolyposis Colorectal Cancer (HNPCC).
HNPCC, also called Lynch syndrome, increases the risk of colon cancer and other cancers. People with HNPCC tend to develop colon cancer before age 50.

Familial Adenomatous Polyposis (FAP)
FAP is a rare disorder that causes you to develop thousands of polyps in the lining of your colon and rectum. People with untreated FAP have a greatly increased risk of developing colon cancer before age 40.
Symptoms
Signs and symptoms of Colorectal cancer may include

Changes in bowel habits, including persistent constipation or diarrhoea, a feeling of not being able to empty the bowel completely, an urgency to move the bowels, or a change in the consistency of the stools ( long, thin "pencil stools")

Rectal bleeding or dark patches of blood in or on stool

Persistent abdominal discomfort such as cramps, bloating, gas or pain

Unexplained fatigue, weakness, loss of appetite and/or weight loss

Pelvic pain, which occurs at later stages of the disease
Risk Factor
Factors that are associated with an increased risk of Colorectal cancer include:

People diagnosed with colon cancer are ofolder age (>50 years). Colon cancer can occur in younger people, but it occurs much less frequently.

Chronic inflammatory diseases of the colon, such as Ulcerative colitis and Crohn's disease, can increase your risk of colon cancer.

Personal history of Colorectal cancer

Family history of colon cancer

Inherited syndromes that increase colon cancer risk.

Sedentary lifestyle

Smoking

Alcohol
Diagnosis
Blood Test
-
Hemogram to check for anemia.
-
Liver enzymes may be checked since colorectal cancer often spread to liver
COLONOSCOPY
-
Most commonly used test to diagnose Colorectal cancer if the symptoms are highly suggestive
BIOPSY
-
Tissue biopsy is taken during colonoscopy from any suspicious area.
-
IHC markers and Genetic tests to be done on the biopsy specimens to identify specific alterations of proteins and gene changes in the cancer cells.
IMAGING TESTS
-
Computed Tomography (CT) scan of liver and other organs
-
Endorectal Ultrasound
-
Magnetic Resonance Imaging (MRI)
-
1Abnormal cells are found in the innermost lining of the colon or rectal wall (mucosa)
-
2Cancer has formed in the mucosa (innermost layer) and has spread to the submucosa (layer of tissue under the mucosa) and muscle layer of colon or rectum
-
3The cancer has grown through the wall of the colon or rectum to the lining of the abdomen, and has grown into nearby structures.
-
4The cancer has grown throught the inner lining or into the muscle layers of the intestine and spread to lymph nodes.
-
In general, screening for colorectal cancer should begin at the age of 45, when the risk for developing colorectal polyps and cancer starts to increase.
-
However, if having a personal or a family history of colorectal polyps or cancer, screening may need to begin before age 45.
-
Men and Women should under screening since colorectal polyps and cancer affect both genders.
-
Discuss with the clinical to ensure what age is best to start your screening based on personal risk factors./p>
Conditions associated with colorectal cancer
-
Polyps: There are a variety of polyps that can form on the inner wall of the colon or rectum. Precancerous polyps can turn into colorectal cancer. People with numerous polypsincluding adenomas, hyperplastic polyps or other types of polypsoften have a genetic predisposition to polyposis and colorectal cancer. These individuals should be managed differently than people with only one to two colorectal polyps.
-
Inflammatory bowel disease: Ulcerative colitis and Crohn's disease are conditions in which the lining of the colon becomes inflamed. People with these conditions, when present for more than seven years and affecting a large portion of the colon, are at greater risk for developing Colorectal cancer.
-
Personal history: A person who already has had colorectal adenomas or cancer may develop the disease a second time. Also, a history of Inflammatory bowel disease can increase the risk of developing Colorectal cancer.
-
Family history: Sometimes colon cancer "runs in" families. This type of moderately increased cancer risk can be called a "familial colon cancer." When a person has a hereditary cancer susceptibility, he or she has inherited a copy of a cancer susceptibility gene with a mutation. Individuals who inherit a mutation in a cancer susceptibility gene have a much greater chance for developing cancer. However, not everyone with a cancer susceptibility gene mutation will develop cancer. Genetic testing is available for all of these colorectal cancer syndromes.




